What Is contact lens allergy?
- December 28, 2021
- by NATALIYA KUSHNIR
- Articles
Since their introduction to the general public in the late 1950s, contact lenses have gained steadily in popularity with advances in lens materials, designs, fitting, and care. Early contacts were made of polymethyl methacrylate (PMMA), a rigid polymer impermeable to the transmission of gases—both the oxygen the cornea consumes as it respires and the carbon dioxide it produces. Moreover, the sensitivity of the eye to lens edges and also to airborne particles meant that many patients could not tolerate their discomfort.
“Soft” lenses made of pliable, water-absorbing polymers became available in 1971 and quickly exceeded hard lenses in popularity. They transmit oxygen relatively well because of their high water content (up to 75 percent in some), and they shape themselves to the cornea, allowing quick adaptation by the eye and increased comfort. Unfortunately, soft lenses, known as hydrogels, are less durable than hard lenses and require greater care and more frequent replacement. With them the eye is more prone to infection and a number of other complications and, while well suited for correcting myopia (nearsightedness), they are often unable to correct astigmatism adequately. Rigid gas-permeable lenses (RGPs), available since 1979, combine good gas transmissibility and the superior optical properties of rigid materials. However, they suffer from some of the same problems as the older PMMA lenses, including greater sensitivity to foreign particles in the eye and increased risk of lens displacement or loss. Both hydrogel and RGP lenses available today offer the possibility of extended wear for periods longer than a day. About a third of the hydrogel lenses in use are of this extended-wear variety (Schein, 1990), with a typical wear time of one week. Nonetheless, all contact lenses, either daily wear or extended wear, must be removed at regular intervals to prevent complications from oxygen deprivation, bacterial infection, and mechanical irritation.What Causes an Allergic Reaction to Contacts?
Contact lens materials
There are two main kinds of contact lenses: soft and gas permeable. Soft contact lenses are made of a plastic polymer and contain at least 10% water. They contribute to more eye infections than rigid or gaspermeable contact lenses. Wearers of these lenses are at a greater risk of developing eye infections and corneal ulcers. These conditions can develop quickly — usually within 24 hours of exposure to the offending agent; they can be very serious and, in rare cases, cause blindness. More is demanded from ophthalmic treatments using contact lenses, which are currently used by over 125 million people around the world. Improving the material of contact lenses (CLs) is a now rapidly evolving discipline. These materials are developing alongside the advances made in related biomaterials for applications such as drug delivery. Contact lens materials are typically based on polymer- or silicone-hydrogel, with additional manufacturing technologies employed to produce the final lens.Contact lens cleansing systems
Multipurpose contact lens solutions are the dominant disinfection method used by contact lens wearers today.What Is Contact Lens Intolerance?
Contact lens intolerance is the same as contact lens discomfort (CLD) that is assessed by ophthalmologists in research. Factors causing CLD can be either contact lens-related or environmental. Contact lens-related factors can be associated with:- material (lubricity, water content),
- design (edge, base curve, asphericity),
- fit,
- wearing schedule,
- care system (chemical composition, regimen).
- ocular surface condition (dry eye, tear composition),
- external environment (humidity, wind, temperature),
- occupational factors (computer, light, altitude, and other occupational related changes in the external environment),
- medications,
- compliance,
- other factors (age, gender, background ocular or systemic diseases, psychiatric and psychological conditions).
Signs That You May Be Allergic to Contacts

What Can I Do to Avoid Irritation?
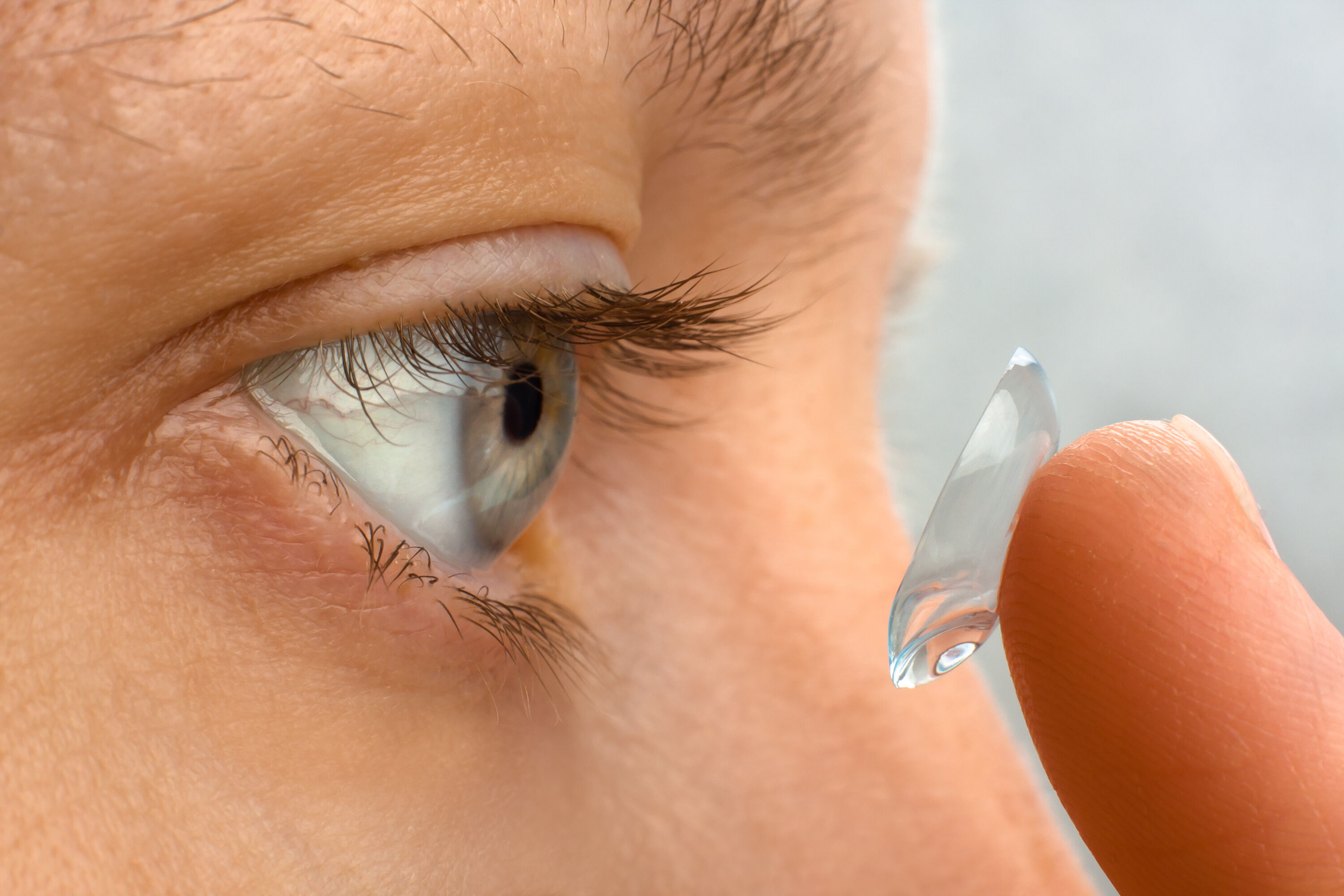
Standard daily-wear soft contact lenses should be cleaned daily. Several professional groups that represent optometrists and ophthalmologists recommend rubbing each lens in the palm of the hand with a few drops of solution, even if using a “no rub” product.
The importance of careful eye care with contacts
Contacts and allergies
Giant papillary conjunctivitis (GPC) can occur with any type of contact lenses. The coating on the lens and the contact lens trauma to the conjunctiva are probable factors. Changing the polymer of the contact lens that a patient with GPC wears can decrease the chance of the condition recurring. Also, replacing a soft contact lens at intervals of less than 3 weeks, rather than 4 or more weeks, significantly reduces the chance of developing GPC. GPC can occur with high Dk silicone contact lenses. Two forms of GPC have been reported: a generalized form similar to that seen with conventional soft contact lenses and a localized form in which the papillae are confined to one or two areas of the tarsal conjunctiva, near the lid margin.Contacts and infections
Improper care of contact lenses can lead to a variety of eye infections including infectious keratitis. Experts in the eye care field agree that estimated rates of microbial keratitis in the contact lens–wearing population has not substantially declined since the first disinfection method using heat, despite the evolution of contact lens disinfection systems.
Treatment
Basic Preventative Steps to Combat Allergies
The modifiable environmental factors should be addressed first. Increasing room humidity, avoiding being in the direction of windy air conditioners, intermittently looking at far objects during computer work, and adjusting the angle of gaze at the computer monitor are simple modifications that can help.

The Importance of Proper Contact Lens Care
While many medications exist, the first and upmost important is to follow all recommendations for the contact lens care. Keeping lens clean and lubricated will help you to wear them without any problems and discomfort. It is only natural to zonk out when a boring doctor is giving you “unnecessary instructions”, but this is not the case for the first-time contacts wearing. We recommend to listen carefully and even take notes, as the doc already saw all possible problems and will give you the best “not to do” recommendations.Eye Drops for Itchy Eyes
Ocular antihistamine drops such as olopatadine and epinastine can decrease symptoms in patients with history of allergic conjunctivitis, even in the absence of symptoms, while oral omega-3 fatty acids can decrease dry eye symptoms.Other Treatments
For the patients who remain symptomatic despite the above-mentioned modifications, a trial of changing the lens type to another with a better surface wettability, and more frequent replacement schedule preferably daily disposable can be helpful.News – a lens delivering medication

